The Journey Begins with Your Eggs
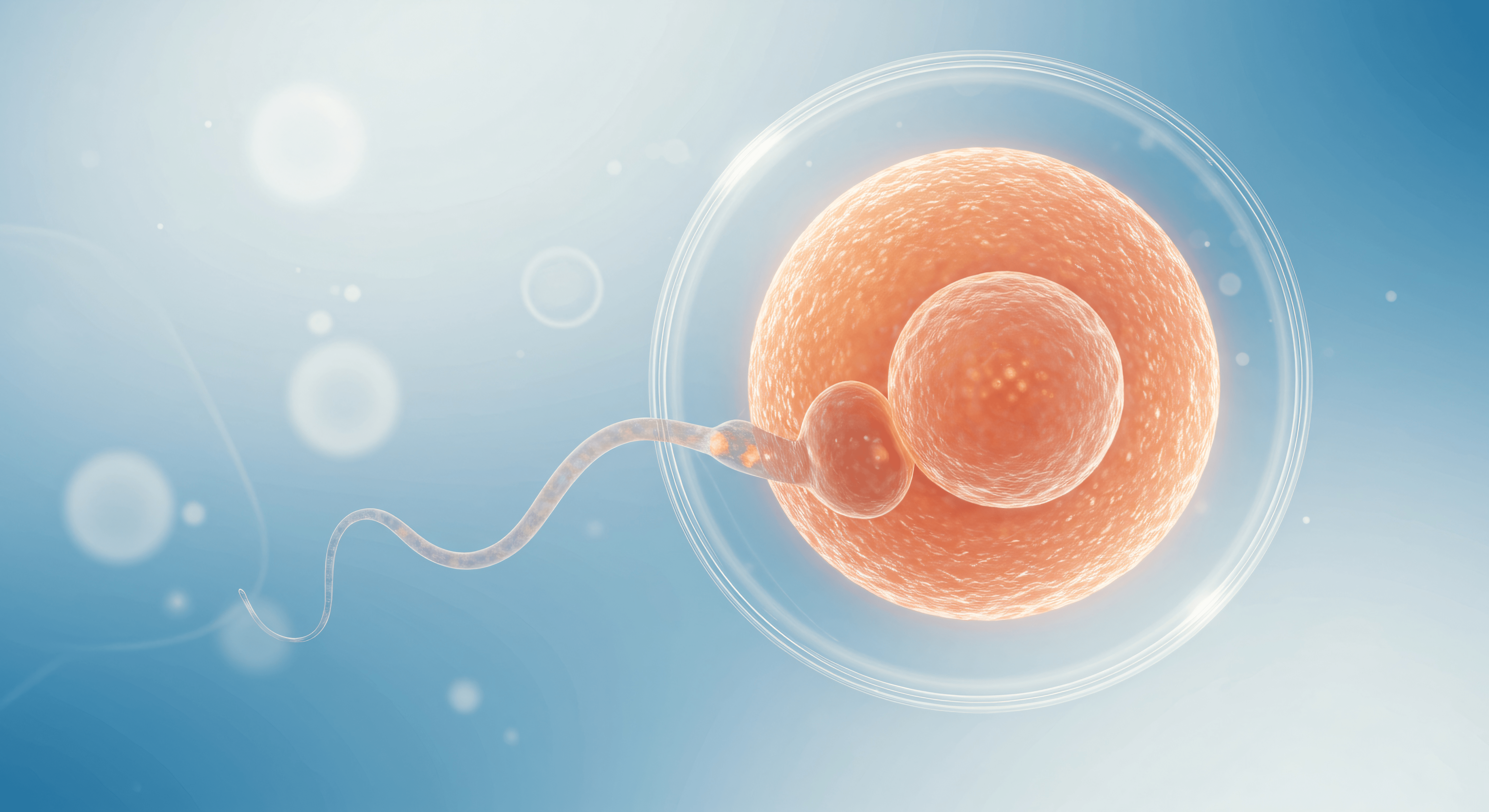
In IVF (in vitro fertilisation), success begins at the very first step: your eggs. While much attention is placed on fertilisation and embryo development, one of the most critical factors influencing IVF success happens earlier—ensuring that the eggs retrieved are mature. But what exactly does it mean for an egg to be “mature,” and why is this so important?
Let’s explore the science of egg maturity, from the early stages in your ovaries to their preparation in the lab.
1. Not All Eggs Are Created Equal: Understanding Oocyte Stages
Human eggs, known as oocytes, develop within fluid-filled sacs in the ovaries called follicles. As follicles grow, the oocytes inside undergo several key developmental stages. By the time of egg retrieval, each oocyte will be at one of the following stages:
Germinal Vesicle (GV):
These are immature oocytes, with a visible nucleus. They haven’t completed the necessary steps for fertilisation and are not viable for use in IVF.
Metaphase I (MI):
These oocytes are partway through maturation but haven’t completed meiosis. While they show some progress, MI eggs are still not ready to be fertilised.
Metaphase II (MII):
This is the gold standard in IVF. MII oocytes have completed the necessary cellular processes and are now ready to be fertilised by sperm.
Only MII-stage oocytes can be fertilised successfully and go on to develop into viable embryos. That’s why achieving maturity is the key focus for both clinicians and embryologists throughout the IVF cycle.


2. Ovarian Stimulation: Encouraging Multiple Eggs to Grow
In a natural menstrual cycle, typically only one follicle matures and releases a single egg during ovulation. However, in IVF, the goal is to collect multiple eggs in one cycle to improve the chances of success. This is achieved through controlled ovarian stimulation using injectable gonadotrophins, such as FSH (follicle-stimulating hormone) and LH (luteinising hormone).
Over the course of 8–14 days, hormone injections encourage the growth of multiple follicles. Your fertility team closely monitors the process with:
Transvaginal ultrasound scans to measure follicle growth
Blood hormone tests, particularly estradiol (E2), which rises as follicles develop
Once the follicles reach optimal size—usually around 18–22 mm—a final injection (commonly known as the trigger shot) is given. This prompt mimics the natural LH surge and helps the oocytes complete the final stage of maturation in preparation for retrieval.
3. Egg Retrieval (Ovum Pick-Up)
Exactly 36 hours after the trigger shot, the egg retrieval (also called ovum pick-up or OPU) is performed. This is a minor surgical procedure done under sedation, typically taking around 15–30 minutes.
A thin needle is guided through the vaginal wall into each follicle using ultrasound guidance, allowing the clinician to aspirate the fluid and, hopefully, retrieve the oocyte within.
However, it’s important to remember that not all retrieved oocytes will be mature. That’s where the embryologists step in.


4. Denudation: Revealing the Egg’s True Stage
Once the eggs are collected, they arrive in the embryology lab surrounded by cumulus cells—a cloud-like cluster of cells that protect and nourish the oocyte during development. To assess each egg’s stage of maturity, the embryology team performs a process called denudation.
Using gentle enzymatic treatment and microscopic tools, the cumulus cells are removed so the egg’s structure becomes fully visible. This allows the embryologist to determine whether the oocyte is in the GV, MI, or MII stage.
Only MII oocytes—those that have completed meiosis I and extruded the first polar body—are selected for fertilisation, typically through ICSI (intracytoplasmic sperm injection).
If conventional IVF is chosen instead, the denudation process is not performed; instead, natural selection determines whether a sperm cell can successfully fertilise the oocyte within the droplet containing the cumulus cells. On the following day, during the fertilisation check, embryologists assess which oocytes have fertilised correctly. For those that have not, the exact reason often remains unknown—though one possible explanation is that the oocyte was not mature at the time of insemination.
5. Why Egg Maturity Matters in IVF
Egg maturity plays a crucial role in determining the outcome of your IVF cycle. Here’s why:
Only mature (MII) eggs can be fertilised by sperm. GV and MI oocytes are biologically incapable of normal fertilisation.
Higher maturity rates improve embryo development rates. The more MII eggs retrieved, the greater your chances of producing high-quality embryos.
Immature eggs may arrest or develop abnormally. Even if immature eggs are injected with sperm, they rarely develop into viable embryos.
This is why embryologists place such importance on accurately identifying and selecting mature eggs. Each mature egg is a potential step closer to creating an embryo—and ultimately, achieving a pregnancy.

6. Can Immature Eggs Ever Be Used?
In some cases, immature oocytes may be placed in culture media to see if they mature in the lab, a process called in vitro maturation (IVM). However, this technique has lower success rates and is not routinely used in standard IVF cycles.
For most patients, focusing on optimising ovarian stimulation and timing egg retrieval correctly remains the most effective way to maximise the number of mature eggs available.
Summary: It’s Not Just About Quantity—It’s About Quality
- After egg retrieval, you may hear a number: “We collected 12 eggs.” But the more important figure is how many of those were mature (MII). Why? Because only mature eggs have the potential to become embryos—and ultimately, a baby.
- By understanding the stages of oocyte development and the steps taken to assess maturity, you can better appreciate the science and precision behind your IVF journey.
- At every stage—from your ovaries to the lab—egg maturity is a defining factor in IVF success.
