The role of the modern human IVF embryologist has evolved significantly since the birth of Louise Brown, the first baby conceived through in vitro fertilization (IVF), in 1978.
Embryology as a discipline has transformed dramatically with the development of increasingly sophisticated technologies, the emergence of IVF solution and equipment commercial manufacturers, automation and technological advancements. These developments have reshaped the daily work lives of embryologists. Here’s a brief overview of how this role has developed over the years and how the daily work has changed over the years.
1978-1980s: The Pioneering Era
Pioneering work by Patrick Steptoe, Robert Edwards and Jean Purdy: Studies leading to the birth of Louise Brown in 1978 marked the beginning of a new era in reproductive medicine. The success of this procedure was due to the pioneering work of embryologists like Jean Purdy, who is considered one of the first embryologists.
Early Techniques: In the early days, embryologists focused on refining the basic techniques of IVF including egg retrieval, fertilisation, and embryo culture. The procedures were labour-intensive, often including also preparation of necessary tools and solutions, as there were no commercial suppliers of IVF products.

1990s: Technological Advancements
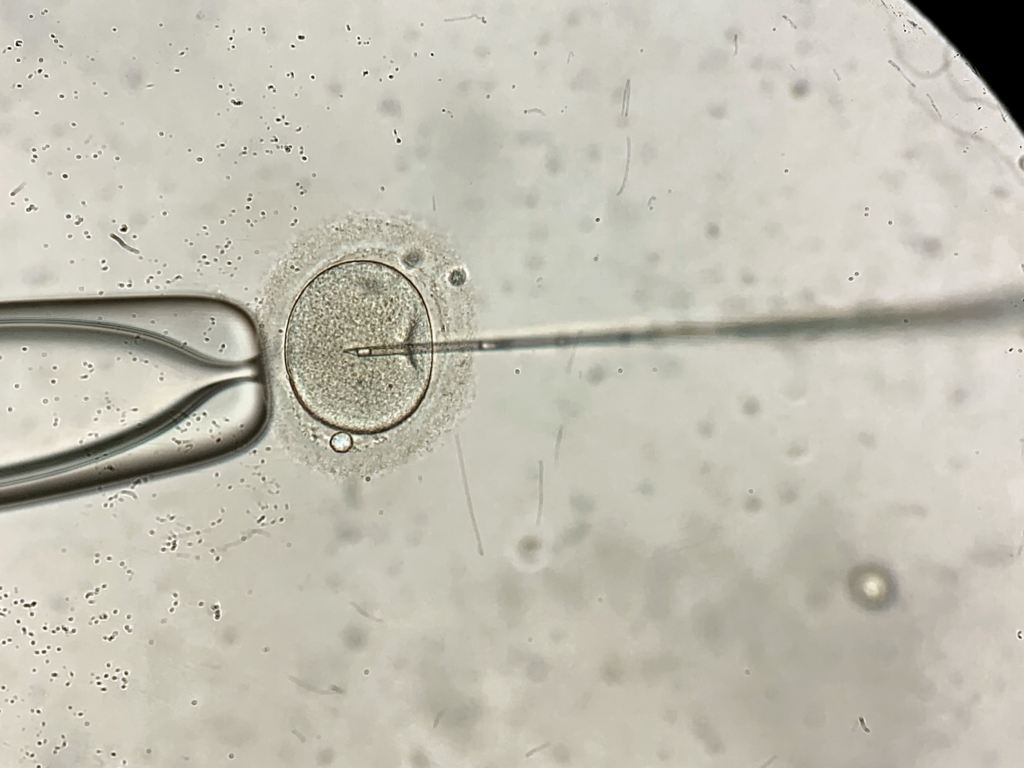
Introduction of ICSI: The 1990s saw the introduction of micromanipulation techniques including intracytoplasmic sperm injection (ICSI), a technique where a single sperm is injected directly into an egg. This advancement required embryologists to develop new skills, but improved success rates for male infertility significantly.
Cryopreservation: Advances in cryopreservation techniques by slow freezing allowed for the freezing and storage of embryos, which provided more flexibility in IVF treatments and increased the chances of successful pregnancies. This, too, require
2000s: Enhanced Culture Systems and Genetic Screening
Improved Culture Media and Incubators: The development of advanced culture media and benchtop incubators improved the quality of embryo culture, leading to higher success rates. These were accompanied by the emergence of suppliers of standardised, ready-made solutions, removing the need for in-house media manufacturing of media, as well as suppliers of specialised IVF incubators. .
Preimplantation Genetic Diagnosis (PGD): Embryologists began using PGD to screen embryos for genetic disorders before implantation, which helped in preventing hereditary diseases. The required embryo biopsy techniques introduced yet another skill requirement for IVF embryologists.
Vitrification: Improved gamete and embryo cryopreservation by vitrification improved success rates but also introduced a new and challenging manual process to the lab, leading to increased demand of highly skilled embryologists.


2010s-Present: Integration of AI and Advanced Imaging
Artificial Intelligence: The integration of AI in embryology is revolutionising the field by its promise of automated and standardised data and image analyses. AI algorithms and software solutions can now be used to assess embryo quality and predict implantation success, making the process more efficient and consistent
Time-Lapse Imaging: Advanced imaging technologies, such as time-lapse microscopy, allow embryologists to monitor embryo development continuously without disturbing embryo culture.
Modern Role
Today, embryologists are integral to fertility clinics, handling gametes (eggs and sperm), performing IVF procedures, monitoring embryo development and interacting with the patients. Their work involves a blend of scientific knowledge, technical skills and empathy, as they help individuals and couples achieve their dreams of parenthood. Despite some of the new technologies seemingly reducing the workload and skills requirements of embryologists, their role continues to be integral. Some of the advantages of recent developments lie in allowing embryologists to focus on tasks requiring human touch while relieving them from routine and monotonous tasks.
Embryologists’ everyday work practices have been shaped significantly by modern technologies, and this trend is likely to continue as these technologies are adopted more widely and developed further. Some comparisons of the past and present changed work practices include:
Before Automation: The Manual Era
- Embryo Observation: Embryologists checked embryos manually under a microscope at specific intervals, briefly exposing them to external conditions.
- Big Box Incubators: Labs relied on traditional incubators with one big temperature and gas-controlled chamber where several patients’ embryos were cultured together, causing exposure to external elements at every door opening.
- Embryo Selection: Decisions were based on a visual snapshot of embryo development at times fitting laboratory workflow and daily routines. This provided minimal and subjective information, making it harder to predict which embryos were the best ones for implantation.
- Data Recording: All observations and results were recorded manually and logged by hand, resulting in vast quantities of paper-based documentation with limited accessibility beyond its storage location.
- Witnessing: Manually double witnessing of procedures requires the presence of minimum of two embryologists in the lab at all times. It caused many interruptions to the embryologists’ workflows increasing the risk of human error.
Before Automation: The Manual Era
- Time-lapse Incubators: Continuous monitoring and recording of embryo development allows embryologists to track embryo development throughout their culture period without disturbing them. More information leads to better decision making.
- Stable Environment: While providing more information, timelapse incubators maintain optimal gas, humidity and temperature environment without disturbances, reducing stress on embryos.
- AI-Assisted Embryo Selection: Artificial intelligence allows embryo assessment in repeatable and consistent manner, helping to identify the most viable embryos based on developmental patterns.
- Digital Data Management: Daily laboratory operations, observations and results are recorded electronically, streamlining workflow and minimising mistakes, and maintaining an accessible record for auditing, KPI tracking, traceability and research purposes.
- Witnessing: Unbiased electronic witnessing allows double witnessing to occur without interrupting another embryologist, and provides an unbroken chain of traceability of all steps of any given process.
- Reduced Burnout: Automation alleviates repetitive tasks, allowing embryologists to focus on complex procedures and patient care.
Impact of Changing Work Practices on IVF Success Rates
- Improved Embryo Viability: Time-lapse imaging and AI-driven selection enhance implantation success.
- More Efficient Workflow: Automation speeds up processes, reducing delays and increasing lab efficiency.
- Reduction in Errors: Allows embryologist to focus on the science.
Automation and technological advancements have revolutionized the science behind embryology, making IVF procedures more efficient and precise. These advancements have also reduced stress on both embryologists and the embryos they grow.
